Although there is no specific or singular clinical symptom or sign for any brain tumors, the presence of a combination of symptoms and the lack of corresponding clinical indications of infections might be an indicator to step up the diagnostic investigation to the direction of an intracranial neoplasm.
The diagnosis will often start with an interrogation of the patient to get a clear view of his medical antecedents, and his current symptoms. Clinical and laboratory investigations will serve to exclude infections as cause of the symptoms. Examinations in this stage may include ophtamological, otolaryngological (or ENT) and/or Electrophysiological exams, other means such as electroencephalography (EEG) play a role in the diagnosis of brain tumors.
Swelling, or obstructing the passage of cerebrospinal fluid (CSF) may cause (early) signs of increased intracranial pressure which translates clinically into headaches, vomiting, or an altered state of consciousness, (and in children) changes to the diameter of the skull and bulging of the fontanelles. More complex symptoms such as endocrine dysfunctions should alarm doctors not to exclude brain tumors.
A bilateral temporal visual field defect (due to compression of the optic chiasm) or dilatation of the pupil, and the occurrence of either slowly evolving or the sudden onset of focal neurologic symptoms, such as cognitivebehavioral impairment (including impaired judgment, memory loss, lack of recognition, spatial orientation disorders), personality or emotional changes, hemiparesis, hypoesthesia, aphasia, ataxia, visual fieldfacial paralysis, double vision, but also more severe symptoms might accur too such as: tremors, paralysis on one side of the body hemiplegia, but also (epileptic) seizures in a patient with a negative history for epilepsy, impairment to swallow should raise red flags. and impairment, impaired sense of smell, impaired hearing,
Imaging plays a central role in the diagnosis of brain tumors. Early imaging methods —invasive and sometimes dangerous— such as pneumoencephalography and cerebral angiography, have been abandoned in recent times in favor of non-invasive, high-resolution techniques, such as computed tomography (CT)-scans and especially magnetic resonance imaging (MRI). Neoplasms will often show as differently colored masses (also referred to as processes) in CT or MRI results.
- Benign brain tumors often show up as hypodense (darker than brain tissue) mass lesions on cranial CT-scans. On MRI, they appear either hypo- (darker than brain tissue) or isointense (same intensity as brain tissue) on T1-weighted scans, or hyperintense (brighter than brain tissue) on T2-weighted MRI, although the appearance is variable.
- Contrast agent uptake, sometimes in characteristic patterns, can be demonstrated on either CT or MRI-scans in most malignant primary and metastatic brain tumors.
- Perifocal edema , or pressure-areas, or where the brain tissue has been compressed by an invasive process also appears hyperintense on T2-weighted MRI, they might indicate the presence a diffuse neoplasm (unclear outline)
This is because these tumors disrupt the normal functioning of the blood-brain barrier and lead to an increase in its permeability. However it is not possible to diagnose high versus low grade gliomas based on enhancement pattern alone.
Another possible diagnostic indicator would be neurofibromatosis which can be in type one or type two.
Glioblastoma multiforme and anaplastic astrocytoma have been associated in case reports on PubMed[who?]porphyrias (PCT, AIP, HCP and VP), including positive testing associated with drug refractory seizures. Unexplained complications associated with drug treatments with these tumors should alert physicians to an undiagnosed neurological porphyria. with the genetic acute hepatic
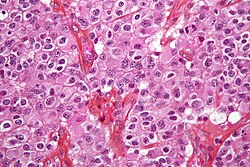
The definitive diagnosis of brain tumor can only be confirmed by histological examination of tumor tissuebiopsy or open surgery. The histological examination is essential for determining the appropriate treatment and the correct prognosis. This examination, performed by a pathologist, typically has three stages: interoperative examination of fresh tissue, preliminary microscopic examination of prepared tissues, and followup examination of prepared tissues after immunohistochemical staining or genetic analysis. samples obtained either by means of brain
 12:59 AM
12:59 AM
 kotesh
kotesh